weight of all organs in human body pdf

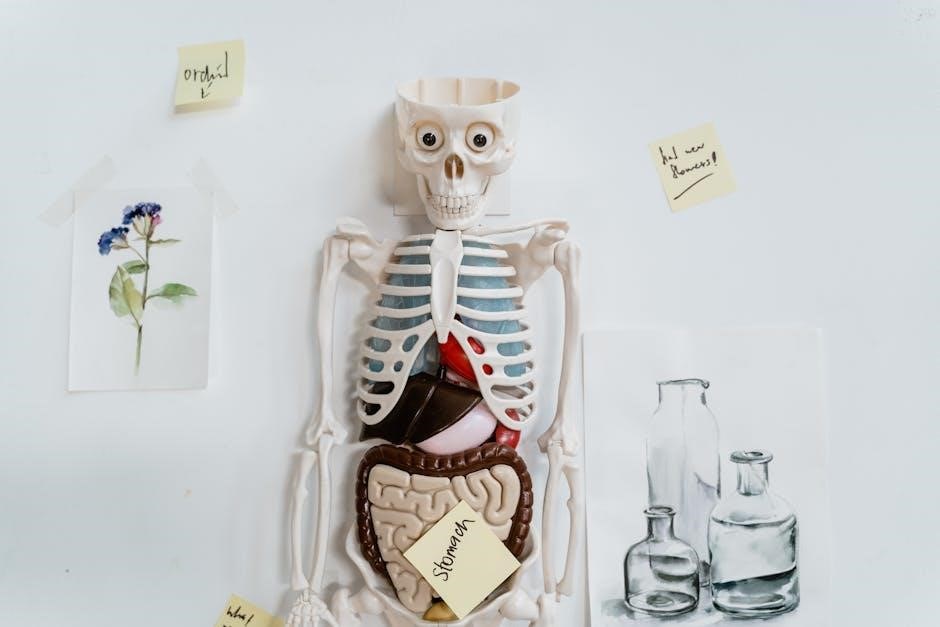
Organ weight plays a crucial role in medical diagnostics and forensic pathology, providing insights into human health and disease processes. Understanding normal organ weights helps identify abnormalities, while variations due to factors like age, gender, and body size highlight the complexity of human anatomy. This article explores the significance of organ weight, its measurement, and its applications in modern science.
1.1 Importance of Organ Weight in Medical and Forensic Sciences
Organ weight is a critical indicator in both medical and forensic sciences, helping to distinguish normal from abnormal conditions. In clinical medicine, it aids in diagnosing diseases, while in forensic pathology, it provides clues about the cause of death. Deviations from normal organ weights can signal underlying health issues or traumatic injuries. Accurate reference tables are essential for comparisons, though outdated data may not reflect modern body habitus changes. Organ weight analysis is vital for understanding disease processes and ensuring precise medical or legal conclusions. This data is increasingly relied upon to improve diagnostic accuracy and inform research, making it a cornerstone of modern scientific investigation.
1.2 Overview of the Human Body’s Organ System
The human body is composed of a complex network of organs, each serving unique functions essential for survival. Major organs include the brain, heart, liver, lungs, kidneys, spleen, pancreas, and skin. The liver is the heaviest internal organ, weighing approximately 1,500 grams, while the brain averages 1,300 grams. Organs like the heart and lungs vary in weight between individuals, with the heart typically around 310 grams and lungs averaging 500 grams. These organs work together to maintain bodily functions, such as circulation, respiration, digestion, and metabolism. Understanding their structure and weight is crucial for medical diagnostics and forensic analysis, as deviations from normal weights can indicate health issues or pathological conditions. This overview provides a foundation for exploring the specific weights and roles of each organ in subsequent sections.

Average Weight of Major Organs in the Human Body
This section provides detailed insights into the average weights of key organs, including the brain, heart, liver, lungs, kidneys, and more, based on forensic and medical data.
2.1 Brain Weight and Its Significance
The human brain typically weighs around 1,300-1,500 grams, accounting for approximately 2% of total body weight while consuming 20% of the body’s energy expenditure. This organ is crucial for controlling voluntary movements, managing sensory information, and facilitating thought processes and emotions. Variations in brain weight can be influenced by factors such as age, gender, and overall health conditions. For instance, studies have shown that brain weight tends to decrease with advancing age, which can be associated with cognitive decline in certain cases. In forensic pathology, brain weight is often analyzed to detect abnormalities that may indicate underlying diseases or trauma. Thus, understanding brain weight is essential for both medical diagnostics and neurological research.
2.2 Heart Weight and Its Comparison to Other Organs
The average weight of a human heart is approximately 250-300 grams, though this can vary based on overall health and body size. Compared to other organs, the heart is significantly lighter than the liver, which is the heaviest internal organ, but slightly heavier than the lungs. The heart’s weight is also less than the brain, which averages around 1,400 grams. Despite its relatively modest size, the heart plays a critical role in circulating blood throughout the body. In forensic and medical contexts, heart weight is often analyzed to assess cardiovascular health, as conditions like hypertension can cause it to enlarge. On average, the heart accounts for about 0.5% of an adult’s total body weight, making it a vital yet proportionally small organ.

2.3 Liver Weight and Its Role as the Heaviest Internal Organ
The liver is the heaviest internal organ in the human body, with an average weight of approximately 1.5 kilograms (3.3 pounds) in adults. This accounts for roughly 2-3% of total body weight. Its substantial size reflects its critical functions, including detoxification, metabolism, and blood filtration. Compared to other organs, the liver outweighs the brain, heart, and lungs, underscoring its vital role in overall health. Variations in liver weight can occur due to factors like body size, hydration levels, and health conditions such as fatty liver disease or cirrhosis. In forensic and medical examinations, liver weight is often measured to assess organ health and detect abnormalities. Its prominence makes it a focal point in clinical diagnostics and research, highlighting its importance in maintaining bodily functions and metabolic balance.

2.4 Lung Weight and Its Variation in Men and Women
The lungs are not the heaviest organs, but their weight varies between individuals and genders. On average, a pair of healthy lungs weighs approximately 1.3 kilograms (2.9 pounds) in men and 1.2 kilograms (2.6 pounds) in women. This difference is attributed to variations in body size and muscle mass. Lung weight can fluctuate due to factors like inflation, blood content, and overall health. For instance, lungs are lighter when deflated and heavier when fully inflated. These weights are general averages, and individual variations may occur based on age, ethnicity, and physical condition. Understanding these differences is crucial for medical diagnostics and forensic analyses, where lung weight can provide insights into health status and potential pathologies.
2.5 Kidney Weight and Its Relevance in Medical Diagnostics
The average weight of a human kidney is approximately 125-170 grams for each organ, with both kidneys combined weighing around 250-340 grams. This weight can vary slightly based on age, gender, and overall body size. Men generally have slightly heavier kidneys than women, which may be attributed to differences in muscle mass and body composition. In medical diagnostics, kidney weight is a critical factor in assessing organ health. For instance, enlarged kidneys may indicate conditions like nephritis or polycystic kidney disease, while reduced weight could suggest chronic kidney disease or ischemia. Accurate measurement of kidney weight is essential in nephrology for evaluating organ function and guiding treatment plans. This data is also valuable in forensic pathology and transplantation medicine.
2.6 Spleen Weight and Its Functional Implications
The average weight of the human spleen is approximately 150-200 grams, though this can vary depending on age, gender, and overall health. The spleen plays a vital role in filtering the blood, storing red blood cells, and supporting the immune system. Its weight can fluctuate due to factors like hydration levels, inflammation, or disease. In medical diagnostics, spleen weight is often assessed to detect conditions such as splenomegaly (enlarged spleen), which may result from infections, liver disease, or blood disorders. Conversely, a smaller-than-average spleen could indicate atrophy or reduced function. Accurate measurement of spleen weight is crucial for understanding its functional status and guiding clinical interventions.
2.7 Pancreas Weight and Its Importance in Metabolism
The average weight of a healthy adult pancreas is approximately 70-100 grams, varying slightly between individuals. This organ is crucial for metabolism, producing digestive enzymes and hormones like insulin and glucagon to regulate blood sugar levels. The pancreas plays a dual role: its exocrine function aids digestion, while its endocrine function controls glucose metabolism. Factors such as age, body size, and health conditions can influence pancreas weight. For instance, pancreatitis or diabetes may alter its mass. Accurate measurement of pancreas weight is essential in clinical settings to diagnose disorders and monitor treatment efficacy. Understanding its weight and function provides insights into metabolic health and disease management.
2.8 Skin Weight and Its Contribution to Total Body Weight
The skin is the heaviest organ in the human body, accounting for approximately 4-5 kilograms (8.8-11 pounds) of an adult’s total body weight. This makes it a significant contributor to overall weight, often overlooked due to its external nature. The skin’s weight varies based on factors like body size, hydration levels, and health conditions. For example, individuals with higher body mass or excess fluid retention may have heavier skin. Conditions like edema can also increase skin weight temporarily. Interestingly, the skin’s weight decreases with age as it loses elasticity and thickness. Despite its weight, the skin plays a vital role in protecting the body, regulating temperature, and aiding in sensory functions. Understanding its contribution helps in assessing overall health and body composition.

Factors Influencing Organ Weight
Organ weight is influenced by body composition, overall health, and genetics, with variations occurring due to age, gender, and lifestyle factors.
3.1 Body Weight and Its Impact on Organ Mass
Body weight significantly influences organ mass, as heavier individuals typically have larger organs to support their greater body mass. For example, the liver and heart may be heavier in individuals with higher body weight to accommodate increased metabolic and circulatory demands. Additionally, fat distribution plays a role, with visceral fat around organs like the liver and pancreas potentially leading to organ enlargement. This relationship is not entirely linear, as muscle mass and overall body composition also affect organ size. Consequently, understanding the correlation between body weight and organ mass is crucial for medical diagnostics and forensic analyses, where normal ranges for organ weights are often adjusted based on an individual’s overall size and body composition.
3.2 Gender Differences in Organ Weight
Gender differences in organ weight are noticeable, with men generally having larger organs than women due to greater overall body size. Organs like the heart and liver are typically heavier in men, aligning with higher muscle mass and body weight. Conversely, women have smaller organ masses on average, though exceptions exist, such as the uterus and breasts, which are larger in women. Hormonal influences, like testosterone promoting muscle growth in men and estrogen affecting fat distribution in women, contribute to these differences. Medical professionals consider these gender-specific variations in diagnostics and autopsies to ensure accurate assessments and maintain patient-specific care standards.
3.3 Age-Related Changes in Organ Weight
Age significantly influences organ weight, with notable changes occurring throughout life. At birth, organs like the brain and liver are proportionally large, reflecting their critical roles in early development. During childhood and adolescence, organ weights increase steadily, reaching peak mass in adulthood. In older adults, certain organs, such as the brain and pancreas, may lose weight due to natural atrophy or reduced cellular density. The liver and kidneys also show age-related declines in mass and functional capacity, which can impact metabolism and detoxification processes. These changes highlight the dynamic nature of organ growth and the importance of considering age when evaluating organ weight in medical diagnostics and research.
3.4 Ethnicity and Geographical Variations in Organ Weight
Ethnicity and geographical location can influence organ weight due to genetic, environmental, and lifestyle factors. Studies suggest that certain populations may exhibit differences in organ mass, potentially linked to evolutionary adaptations or dietary habits. For instance, individuals from regions with higher physical activity levels may have slightly heavier hearts and muscles. Additionally, ethnic variations in body composition, such as differences in lean body mass, can affect organ weights. Geographical factors like altitude and climate may also play a role, as seen in populations living at high altitudes, where lung and heart weights might adapt to lower oxygen levels. These variations highlight the importance of considering demographic factors in medical and forensic assessments of organ weight.
3.5 Lean Body Mass and Its Effect on Organ Weight
Lean body mass (LBM), which includes muscles, bones, and water, plays a significant role in determining organ weight. Individuals with higher LBM tend to have larger organs, as these organs support increased metabolic activity. For example, the heart, liver, and kidneys may be heavier in people with greater muscle mass due to higher energy demands. This relationship is crucial in medical assessments, as it helps establish normal organ weight ranges based on body composition. LBM is influenced by factors like genetics, nutrition, and physical activity, making it a key consideration in understanding organ weight variations. Accurate measurements of LBM can provide insights into how it impacts organ size and function across different populations.
Applications of Organ Weight Data
Organ weight data is crucial in forensic pathology for autopsy analysis and clinical diagnostics to detect abnormalities, aiding medical research, transplantation success, and assessing overall health.
4.1 Role in Forensic Pathology and Autopsy Analysis
Organ weight data plays a vital role in forensic pathology, particularly during autopsies, to determine cause of death and assess overall health. By comparing organ weights to established norms, pathologists can identify abnormalities, such as an enlarged heart in hypertensive individuals or a heavy liver in cases of fatty liver disease. This data also aids in detecting poisonings, as certain toxins affect specific organs, altering their weight. Additionally, organ weight analysis helps estimate the time since death and identifies congenital anomalies. Standardized organ weight databases enable forensic experts to draw accurate conclusions, making it a cornerstone of post-mortem investigations and criminal case resolutions. Its reliability ensures justice and medical understanding.
4.2 Use in Clinical Medicine for Diagnostics
Organ weight data is crucial in clinical medicine for diagnosing various conditions and monitoring disease progression. For instance, an enlarged liver or heart may indicate cirrhosis, cardiomyopathy, or other pathologies. Similarly, abnormal kidney weight can signal chronic kidney disease or hypertension. In surgical settings, organ weight measurements guide transplant evaluations and tumor assessments. Imaging techniques like MRI and CT scans allow non-invasive estimation of organ weight, aiding in early detection of abnormalities. This data also helps in tailoring treatment plans, such as adjusting medication dosages based on organ size. By providing quantitative insights, organ weight becomes a valuable tool for precise diagnostics and personalized patient care, enhancing treatment outcomes and improving public health strategies.

Measuring Organ Weight
Organ weight is measured through autopsy examinations or advanced imaging techniques like MRI and CT scans, ensuring accurate data collection for clinical and research purposes.
5.1 Autopsy-Based Measurement Techniques
Autopsy-based measurement is the gold standard for determining organ weight, offering precise data through direct physical examination. During an autopsy, organs are carefully dissected, and their weights are recorded using highly sensitive analytical balances. This method ensures accuracy, as it eliminates variables like tissue inflation or fluid retention. Pathologists follow standardized protocols to measure organs, ensuring consistency across cases. The process involves weighing each organ individually, with results documented in grams or kilograms. This technique is crucial for research, diagnostics, and forensic investigations, providing reliable data on organ mass. Autopsy-based measurements are also used to establish baseline values for normal and pathological conditions, aiding in the identification of abnormalities. The detailed documentation of organ weights during autopsies contributes significantly to medical knowledge and practice.

5.2 Imaging and Non-Invasive Methods for Estimating Organ Weight
Imaging techniques like MRI, CT scans, and ultrasound are widely used for non-invasive organ weight estimation. These methods provide detailed organ visuals, allowing for precise measurements. By assessing organ dimensions and volume, professionals can calculate weight using established density values. MRI offers high-resolution images, making it ideal for organs like the brain and liver. CT scans are quick and effective for abdominal organs, while ultrasound is portable and commonly used for real-time assessments, especially of the liver and kidneys. These modalities reduce the need for invasive procedures, minimizing risks and enabling repeated monitoring. However, accuracy may vary due to factors like organ shape variability and technician expertise. Despite these limitations, imaging remains a valuable tool in clinical diagnostics and research for estimating organ weight without surgery.

The study of organ weights provides critical insights into human anatomy and physiology, aiding medical diagnostics and forensic investigations. Understanding these weights helps in assessing health conditions, ensuring accurate diagnoses, and advancing research in various scientific fields.

6.1 Summary of Key Findings
The analysis of organ weights reveals significant insights into human anatomy and physiology. The brain, heart, liver, and lungs are among the heaviest organs, with the liver being the heaviest internal organ. Organ weights vary by gender, age, and body composition, influencing their functional capacities. For instance, men generally have heavier organs than women, and organ mass declines with age. These variations are crucial for medical diagnostics and forensic investigations. Understanding organ weights aids in identifying pathologies, such as enlarged hearts or livers, and informs surgical and autopsy practices. Additionally, advancements in imaging techniques have improved non-invasive organ weight estimation, enhancing clinical accuracy. These findings underscore the importance of organ weight data in advancing medical science and personalized healthcare strategies.
6.2 Future Directions in Organ Weight Research
Future research on organ weight should focus on advancing non-invasive measurement techniques, such as enhanced MRI and CT scans, to improve accuracy and accessibility. Artificial intelligence could play a role in analyzing organ weight data, enabling better predictions and personalized health assessments. Additionally, studies should explore how genetic and environmental factors influence organ weight variability. Expanding datasets to include diverse populations will help establish more comprehensive norms. There is also a need to investigate how organ weight changes in response to chronic diseases and lifestyle factors. Collaborative efforts between researchers and clinicians can lead to standardized protocols for measuring and interpreting organ weight, ultimately enhancing diagnostic and therapeutic outcomes. Such advancements will deepen our understanding of human anatomy and improve healthcare practices globally.